In Their Own Words: How Fragmented Care Harms People with Both Mental Illness and Substance Use Disorder
For the 8.9 million American adults — about 500,000 Californians — with a dual diagnosis of mental illness and substance use disorder, it can be difficult to receive fully coordinated and effective care. For people with low incomes, the barriers can be even higher and lead to unnecessary suffering and poor health outcomes.
To better understand how Californians with dual diagnoses experience treatment, CHCF commissioned interviews with 54 people insured through Medi-Cal who have both mental illness and substance use disorder (SUD), as well as additional interviews with the family members and close friends who support them. The research was conducted by a team with NORC at the University of Chicago, which also interviewed providers, provider administrators, and subject matter experts to provide context and to highlight structural and cultural impediments to care.
Fragmented Systems Contribute to Poor Health Outcomes
Together, these firsthand stories expose pervasive problems in the health care system, including a care environment that continues to be divided into separate systems — one for mental health treatment and one for substance use disorders, each with its own data and financing mechanisms, charting requirements, and privacy regulations. Physical health care is yet another separate system.
While the siloed care system is cumbersome for patients and providers alike, it also directly contributes to poor health outcomes. This begins as soon as people enter treatment and their presenting symptoms are diagnosed, either as mental illness or substance use disorder but rarely both. The health system’s reliance on this either/or “primary diagnosis” determines not only where people enter care, but how they self-identify moving forward, putting them at risk of relapse or never having their illnesses fully treated.
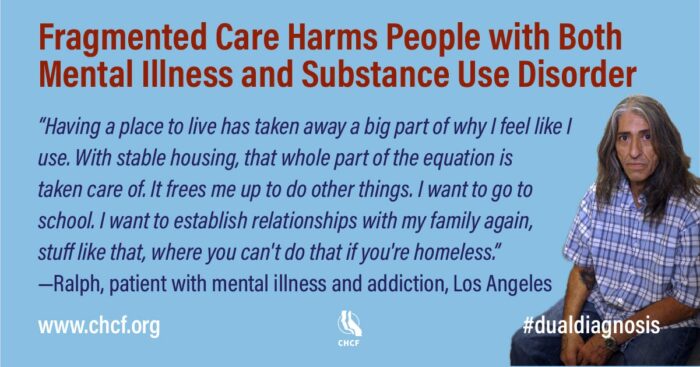
Many Experience Homelessness
A startling finding was the high risk of experiencing homelessness. Many of the 54 people interviewed had had a period of homelessness, sometimes stretching years.
A Clear Solution: Coordinated Care
Yet the report also highlights what works — coordinated care across mental health, substance use, and physical health systems. Many people with dual diagnoses emphasized that they achieved well-being only when all their health care providers worked together, and when other supports were available to them: housing, employment training and placement, and transition from residential treatment or incarceration.
In the full report, interviewees are not identified by name; however, four people agreed to participate in videos and share their personal stories. Click on the images below to see “Rosalind’s Story: Living with Serious Mental Illness and Alcoholism” and “In Their Own Words: People with Mental Illness and Addiction at Risk for Homelessness.”
Posted August 23, 2021, by CHCF
Authors: Susan Anthony, Rebecca Catterson (NORC), Suzanne Campanella (NORC)